Uterine Anomalies
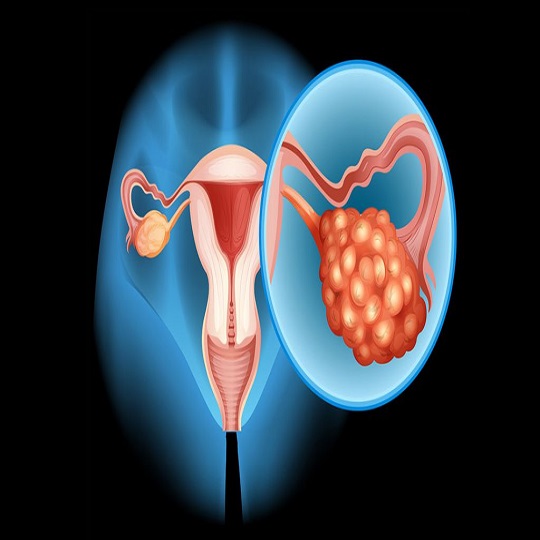
Uterine anomalies refer to various structural or morphological disorders that affect the normal development of the female reproductive system. While in the womb, the uterus of female babies begins to develop as two separate halves. When it completes its development, these two separate parts are fused together and the separator in between is separated, forming a whole. However, in some female babies, disruptions that may occur during this development process may lead to deformities in the uterus. These deformities that occur in the uterus are called uterine anomalies.
Congenital uterine anomalies are seen in less than 5% of all women, but it has been observed that this rate can increase to 25% in women who have miscarriages and/or give birth to premature babies.
Uterine anomalies can usually be congenital, but they can also be caused by factors such as infections, trauma or surgical interventions. These anomalies can have significant effects on women’s reproductive health and in some cases can cause pregnancy problems.
Female Reproductive System and Uterine Anatomy
The uterus is an important part of the female reproductive system. The uterus is designed to carry and grow the fetus during pregnancy. Normally, the uterus develops with a natural curvature and in a certain way. However, for various reasons, this development may deviate from normal and uterine anomalies may occur.
Classification of Uterine Anomalies
Uterine anomalies can be classified according to congenital deformities or acquired adhesions within the uterus. This classification is important for the diagnosis and treatment of the disease.
Deformities: The uterus may develop differently than normal. These deformities are usually congenital. Septate and bicornuate uterus are the most common deformities. Common deformities:
Septate uterus: The uterus is a single whole from the outside, but there are 2 endometrial cavities inside.
Bicornuate uterus: There is an outer surface of the uterus that is indented like a double horn, resembling a heart shape, and 2 endometrial cavities on the outer surface.
Arcuate uterus: There is a normal outer uterine surface that is indented 1 cm or less into the endometrial cavity.
Unicornuate uterus: only one half of the uterus is developed.
Didelphys: the two halves of the uterus remain separate. The patient has a double uterus and a double cervix.
Adhesions in the Uterus: This refers to adhesions on the inner surface of the uterus. Adhesions in the uterus can cause pain during menstrual periods and prevent the normal flow of menstrual blood. It can also lead to problems such as infertility.
Causes and Symptoms of Congenital Uterine Anomalies
In most cases, the cause is unknown. Most women with uterine anomalies have normal chromosome numbers. Diethylstilbestrol (DES), which was used to prevent miscarriage and premature birth between 1938 and 1971, was found to increase congenital uterine anomalies in the babies of these women.
Congenital anomalies are often detected incidentally. They usually do not cause any complaints in the patient. Some women may experience painful menstruation, difficulty conceiving, premature birth or recurrent miscarriages.
Diagnostic Methods
A detailed medical history and detailed examination taken from the patient may suggest a uterine anomaly in the diagnosis. However, gynecological ultrasonography, Magnetic Resonance Imaging (MRI) and hysterosalpingography (HSG) are helpful imaging methods in making the diagnosis. In addition, the type of uterine anomalies can be understood and some can be treated during hysteroscopy and laparoscopy, which are minimally invasive methods.
These diagnostic methods play an important role in diagnosing and determining the degree of uterine anomalies. Doctors can decide which imaging method to use based on the patient’s condition and symptoms.
Causes of Uterine Anomalies
There are several factors that affect the formation of Uterine Anomalies:
Congenital Factors and Genetic Predisposition
Most uterine anomalies occur during the embryonic period before birth and are caused by genetic factors. The genetic makeup of the mother or father can affect some of the determining factors in uterine development. For example, a parent or family member having uterine anomalies can be an indicator of genetic predisposition. Genetic predisposition can affect the normal formation of the uterine shape and structure and, in some cases, can lead to congenital uterine anomalies.
Uterine Infections and Inflammation
Uterine infections or inflammations can damage the uterus and surrounding tissues and affect the structure of the uterus. Infections usually occur as a result of sexually transmitted diseases (Sexually Transmitted Infections – STIs) or other bacterial infections. These infections can damage the uterine tissue and structural components within the uterus and, over time, lead to uterine anomalies.
Causes of Adhesions in the Uterus
Adhesions in the uterus can cause the uterine walls to stick together or create an adherent area. These adhesions usually occur after inflammatory conditions or surgical interventions in the uterus. For example, intrauterine adhesions can develop after an abortion or intrauterine surgery. Intrauterine adhesions can affect the normal menstrual cycle and lead to problems such as infertility.
Hormonal Imbalances and Uterine Anomalies
Hormonal imbalances can affect the development and structural integrity of the uterus. Especially during periods of hormonal changes such as puberty or menopause, hormonal effects on the uterine tissue can become apparent. Hormonal imbalances can affect the thickness of the endometrium and lead to structural disorders in the uterus. These conditions can contribute to irregular menstrual cycles and the formation of some uterine anomalies.
These factors are various factors that play an important role in the formation of uterine anomalies. Each condition can affect the structural integrity of the uterus, causing a variety of anomalies. Treatment and management strategies are usually directed at these underlying causes and are individualized depending on the patient’s condition and symptoms.
Treatment of Uterine Anomalies
There is no nonsurgical treatment for uterine anomalies. When deciding on surgical treatment, it is important to evaluate the type, degree, obstetric history and complaints of the woman in detail. In mild uterine anomalies, if there is no poor obstetric history such as recurrent pregnancy losses, no intervention is usually required. If a septate uterus is detected during infertility and/or pregnancy loss evaluation, surgical treatment is usually recommended. Bicornuate, unicornuate and didelphic uterus rarely require surgical treatment.
Many women with congenital uterine anomalies do not have any medical or fertility problems. However, this condition may slightly increase the woman’s chances of miscarriage or premature birth. If a woman has a septate uterus and has had a miscarriage, surgical treatment may increase her chances of a successful pregnancy.
Surgical Approach
Hysteroscopy: Hysteroscopy is a surgical procedure used to observe and treat intrauterine structures. A thin tube called a hysteroscope and a camera are placed inside the uterus and images are obtained. This method can also be used to open adhesions or septums inside the uterus or to correct structural disorders.
Laparoscopy: Laparoscopy is a surgical technique used to observe the inside of the abdomen by inserting a thin camera into the abdominal cavity through the navel. Laparoscopy can be used to diagnose uterine anomalies and perform surgical interventions. Laparoscopic surgery may be preferred especially for the correction of structural anomalies in the uterus.
Healing Process and Monitoring of Uterine Anomalies After Treatment
Healing Process: The healing process after surgical interventions usually depends on the patient’s health status, the type of operation and whether there are any complications. Rest, appropriate pain management and other treatments recommended by the doctor are important during the healing process.
Monitoring and Follow-up: Monitoring and follow-up of uterine anomalies after treatment is important. Assoc. Esra ÖZBAŞLI, they may perform examinations and imaging tests to regularly evaluate the patient’s health status. This monitoring process is important to evaluate the effectiveness of treatment and detect possible complications early.