Genital Wart (Genital Condyloma, Condyloma Akuminatum)
Genital Warts | Genital warts are the most common type of sexually transmitted disease. They are usually skin lesions that appear on the skin or mucosa.
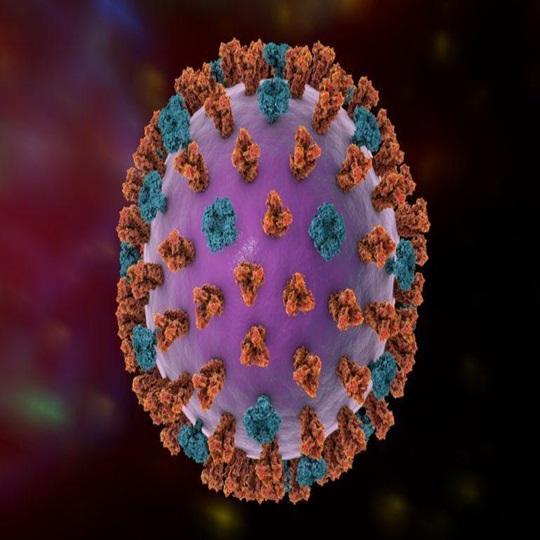
They occur as a result of HPV (Human Papillomavirus) infection. Genital warts are most commonly associated with HPV types 6 and 11.
Warts tend to appear in the genital area, especially the vagina, anus and surrounding skin.
Transmission and Spread: Warts tend to be transmitted through sexual contact and are therefore among the sexually transmitted diseases.
Symptoms and Complications: Warts can sometimes be associated with symptoms such as itching, burning or bleeding and in some cases can develop into precancerous lesions.
Treatment Approach: It usually depends on the size and location of the lesions and the general health of the patient. Treatment options may include freezing (cryotherapy), surgical removal, medical treatment, laser application, chemical applications.
Condyloma Transmission Routes and Risk Factors
Sexual Contact: Condyloma is usually transmitted through sexual contact. The HPV virus can easily pass from intact skin or mucosa to the skin or mucosa of an infected person. The risk of transmission is especially high through genital, anal and oral sex.
Number of Sexual Partners: People who have more than one sexual partner, especially those who have unprotected sex, are at higher risk of developing condyloma. Because each new partner can increase the risk of infection.
Conditions at Risk of Being Infected with HPV: People with weak immune systems, especially HIV-positive individuals, those taking drugs that suppress the immune system or those receiving immunosuppressive therapy after organ transplantation, are more vulnerable to HPV infection and therefore have a higher risk of developing condyloma.
Smoking: Smoking can increase the risk of HPV infection and therefore the development of condyloma. Smoking has negative effects on the immune system, which can weaken the body’s defenses against viral infections.
Sex Education and Awareness: Lack of sexual education or incorrect information can increase the risk of contracting condyloma. Having the right information is important to protect yourself from sexually transmitted infections.
History of Condyloma: People who have had condyloma before may have an increased risk of recurring infections. Therefore, it is recommended that people with a history of condyloma be checked regularly.
Which HPV Types Cause Condyloma?
HPV 6 and HPV 11: The majority of condylomas, especially genital condylomas, are associated with HPV types 6 and 11. These types are known as low-risk HPV types and are usually benign lesions. HPV 6 and 11 condylomas are usually transmitted through sexual contact.
Other Low-Risk HPV Types: Other low-risk HPV types can also rarely cause condylomas. These include HPV types 42, 43, 44, 54, and 61. However, HPV 6 and 11 are the most common causes of condylomas.
High-Risk HPV Types: In some cases, high-risk HPV types can also cause condylomas, but this is rare. High-risk HPV types are associated with cancers, especially cervical cancer, while condylomas are usually associated with low-risk types.
Genetic and Environmental Factors: HPV transmission may also depend on a person’s genetic predisposition and environmental factors
Symptoms and Diagnosis of Condylomata: Condylomata usually appear as small, tag-like growths on the genital area or the skin around the anus. However, they can sometimes be asymptomatic. Diagnosis is made through physical examination and sometimes tests to detect HPV.
Duration and Methods of Condyloma Treatment
Treatment Duration: The duration of condyloma treatment varies depending on factors such as the size and location of the lesions and the patient’s immune system. The treatment period usually varies from weeks to several months. A single treatment session may be sufficient, but sometimes repeated sessions may be required.
Treatment Methods:
Cryotherapy (Freezing): This is the process of freezing the lesions using a cooling agent such as liquid nitrogen. This method is frequently used in the treatment of small condylomas.
Chemical Treatments: Chemical substances such as podophyllin, podophyllotoxin or trichloroacetic acid can be used to burn or destroy condyloma lesions.
Surgical Removal or Burning Treatment: Surgical methods can be applied to remove large or resistant condyloma lesions. This can be done with methods such as electrocautery or laser surgery. It can also be destroyed by burning with electrocautery or laser.
Immunotherapy: Genital Warts | This is a treatment method that helps the body naturally destroy condylomas by stimulating the immune system. This can be done with medications such as interferon drugs or imikvimod cream.
Topical Treatments: Genital Warts | Topical creams can also be used to treat condylomas. These creams are usually designed to kill the HPV infection or stop the lesions from growing.
Post-Treatment Follow-up: Genital Warts | Regular check-ups are important after treatment to check if the lesions have returned. Post-treatment follow-up is necessary to ensure that the infection has been completely cleared.
Partner Treatment: Since it is a sexually transmitted infection, it is important to treat the sexual partners of an infected person as well. This can help prevent the infection from recurring and spreading.
Condyloma Treatment: Although generally effective, there is a risk of recurrence. Therefore, regular follow-up and appropriate precautions are important after treatment.
Genital Warts | The cervical cancer vaccine also protects against HPV types 6 and 11. Therefore, being vaccinated at an early age will minimize the risk of getting condylomas in the future. There are studies in the literature that even if the condyloma is removed, the lesions will be much less. It is recommended that people who have had condyloma are vaccinated. In this way, the vaccine will prevent the HPV from being taken back after it is eliminated from the body.
Assoc. Prof. Dr. Esra Özbaşlı’s Wart-Condyloma Treatment Approach
Individualized Treatment Plan: Genital Warts | Assoc. Prof. Dr. Esra Özbaşlı prefers to create an individualized treatment plan for each patient. Treatment methods are determined by considering factors such as the location, size, number of lesions and the patient’s general health.
A Complete Examination: Genital Warts | Özbaşlı’s approach is based on a complete physical examination and a detailed review of the patient’s medical history. This helps to fully evaluate the patient’s condition and determine the most appropriate treatment plan.
Explanation of Treatment Options: Genital Warts | The patient is provided with detailed information about the available treatment options. The advantages, disadvantages and possible side effects of each treatment option are explained so that the patient can make an informed decision.
Use of Advanced Technology: Genital Warts | Özbaşlı aims to provide the best care to her patients by using the latest technologies and treatment methods offered by contemporary medicine. This allows for the lesions to be detected precisely and treated effectively.
Patient Education and Support: Genital Warts | Patients are provided with accurate information about condyloma infections and are supported throughout the treatment process. Patients are educated, especially on the prevention of sexually transmitted infections, and are made aware of protective measures.
Post-Treatment Follow-up: Genital Warts | After treatment, it is important to regularly check patients and monitor whether the lesions have returned. Özbaşlı meticulously follows up on her patients after treatment and plans additional treatments or interventions when necessary.
Assoc. Prof. Dr. Esra Özbaşlı’s approach aims to provide her patients with the most effective and individualized treatment. In this way, it is aimed for patients to get the best results from the treatment process and prevent recurrence of the infection.